What is Dance Medicine?
Dance medicine is a sub-category of Sports Medicine and involves the direct treatment of dancers and performing artists. This particular population presents with a unique set of needs that need to be addressed by qualified practitioners. Our dance medicine specialists have extensive knowledge of the demands required of dancers and are able to appropriately diagnose injuries as well as provide the most appropriate care. Cynergy’s skilled Dance Medicine clinicians will aid you in achieving optimal performance and help guide you during your recovery back to the stage or classroom.
Who Can Benefit?
It takes a certain type of physical therapist to work with stage performers. That said, our dance medicine specialists have expert knowledge in treating patients of any age and level of expertise. Whether you’re a Broadway performer, preparing for your first show or simply aiming to do your best in dance class, Cynergy’s dance medicine team will help you achieve your goals with a tailored program to address your particular needs
Common Dance Injuries
Muscle strains
A muscle strain, or “pulled muscle”, occurs when a muscle is overstretched or torn due to an intense contraction. This can happen when performing a vigorous or quick activity such as jumping, running, or even everyday tasks. There are different grades of muscle strains that can be diagnosed clinically with imaging. Grade 1 is mild, grade 2 is moderate, and grade 3 is severe. Symptoms of a muscle strain might include swelling, bruising, redness, pain at rest and with movement, and weakness. Physical therapy can help in the reduction of pain and swelling in the acute, or initial phase of the injury. A physical therapist will also educate about how to modify activities to reduce pain and aggravation of symptoms. In the second phase of your injury, your physical therapist can provide you with an exercise program that includes muscle strengthening, balance, and endurance training, as well as use hands-on techniques to aid in both mobility and blood flow to the injured area.
Patellofemoral syndrome
Patellofemoral dysfunction is pain at the front of your knee, around your kneecap (patella). Sometimes called “runner’s knee,” it’s more common in people who participate in sports that involve running and jumping. The knee pain often increases when you run, walk up or downstairs, sit for long periods, or squat. Simple treatments such as rest and ice often help, but sometimes physical therapy is needed to ease patellofemoral pain.
Patellofemoral dysfunction can stem from any of the following:
- Running or jumping sports puts repetitive stress on your knee joint, which can cause irritation under the kneecap.
- Muscle imbalances or weaknesses. Patellofemoral pain can occur when the muscles around your hip and knee don’t keep your kneecap properly aligned. Inward movement of the knee during a squat has been found to be associated with patellofemoral pain.
- Trauma to the kneecap, such as a dislocation or fracture, has been linked to patellofemoral pain syndrome.
- Knee surgery, particularly repair to the anterior cruciate ligament using your own patellar tendon as a graft, increases the risk of patellofemoral pain.
Your physical therapist will work with you to maintain your strength and flexibility as well as optimize your movements with jumping, running, and pivoting, all geared to help keep the patella tracking properly in its groove.
Ankle sprain
Ankle sprains occur when the ligaments that help stabilize your ankle become injured. This may occur when the ankle is excessively turned or rotated, overstretching the ligaments. These overstretched ligaments cause the ankle to lose stability, leading to pain and balance issues. Physical therapy can help by restoring joint range of motion, reducing swelling and edema, strengthening to improve stability, and education on ways to avoid re-injury in the future.
Post-op rehabilitation
Some dance injuries may require surgical correction. These injuries can be a result of a trauma, such as a fall in rehearsal or performance, and occasionally, due to an overuse injury that was not managed conservatively and early enough. Dance injuries that may require surgery and subsequent post-operative management include meniscal tears, ACL tears, PCL tears, ankle fractures, os trigonum excision, labral tears of the shoulder or hip, severe Achilles, and biceps, or patellar tendon tears. Skilled physical therapy will guide you through each phase of post-op rehabilitation, from recovering from the surgery itself in the acute phase to restoring motion and strength to regaining function and finally returning to class and the stage.
Bunions
Bunions, or hallux valgus, are defined as an inward deviation of the great toe towards the 2nd toe, due to an outward splaying of the 1st metatarsal head (or big toe “ball”). Though there may be a hereditary component to developing bunions, there are various factors that may contribute to the development of this condition in dancers. Physical therapy can help by improving intrinsic foot strength and assessing whether undue stress is occurring at the great toe joint through forced turn-out, winging, and poor landing mechanics. By addressing foot strength and mobility as well as other contributing factors, your therapist can devise a plan that can improve your foot function and prevent recurrence and/or progression of this condition.
Stress fractures
A stress fracture is when a small crack occurs in a bone, usually due to high impact activities, overuse, and poor mechanics during exercise. While stress fractures can occur throughout the body, they are most common in the lower extremities, specifically in the shin, ankle, and foot. The first goal of physical therapy is to protect the injury, so it does not turn into a full fracture. Following the protective phase, your therapist will assess and address any range of motion or strength impairments, as well as your mechanics to help prevent the risk of re-injury when returning to your prior activities.
Tendinopathies (upper and lower extremities)
Tendinopathy is a general term used to describe conditions surrounding the overuse of tendons. More specifically, tendinosis is a degeneration of the collagen fibers within the tendon and tendonitis is the overall inflammation of the tendon. Common areas for dancers to experience tendinopathy are the heel, or Achilles, peroneals in the outer ankle, the posterior tibialis in the inner ankle and foot, and the rotator cuff and biceps tendon in the shoulder. Symptoms of tendinosis or tendinitis include local pain and tenderness, pain that radiates above or below the injured area, inflammation, and weakness of the muscle. Physical therapy can help via manual techniques including soft tissue release, stretching, and mobility exercises to restore range of motion, strengthening of the affected muscles and tendons, as well as functional training to restore and improve your dance technique.
Get Back to the Stage Stronger Than Ever
Whether you're recovering from an injury, preparing for a performance, or looking to prevent future setbacks, our Dance Medicine team is here to support you every step (and leap) of the way. With personalized care from clinicians who understand the unique demands of dance, we’ll help you move, perform, and feel your best.
👉 Schedule Your Dance Medicine Evaluation Today
Let’s get you back to doing what you love—with confidence and strength.
📞 Call us at 212- 255-8080, 212-980-2963, or 212-292-7117
Meet our Dance Medicine Specialists

Laurence Agénor, PT, DPT, CSCS specializes in performance, dance medicine, and Pilates. As a dancer, she has a unique understanding of the dancer’s body and what it means to perform at an optimal level. Her holistic treatment approach blends her background as a dancer and movement specialist with her clinical expertise. She enjoys working with dancers of all ages, levels, and backgrounds and believes in empowering her clients with the knowledge and skills they need to propel their performance forward.


Born and raised in Salt Lake City, Utah, Lindsay Ryan discovered her passion for dance and the outdoors. Her desire to dance professionally drew her to San Francisco where she attended Saint Mary’s College of California. During her time on the west coast, Lindsay spent several years dancing for companies in the Bay Area. Eventually, she applied to the NYU DPT program and melded her passion for movement and science. Lindsay continued to dance while pursuing her doctorate in Physical Therapy. She has appeared in dance films, teaches various dance styles, and is currently a commercial and entertainment performer.
Lindsay is dedicated to enhancing the quality of movement for her patients and is excited to showcase the transformative potential of rehabilitation at Cynergy.
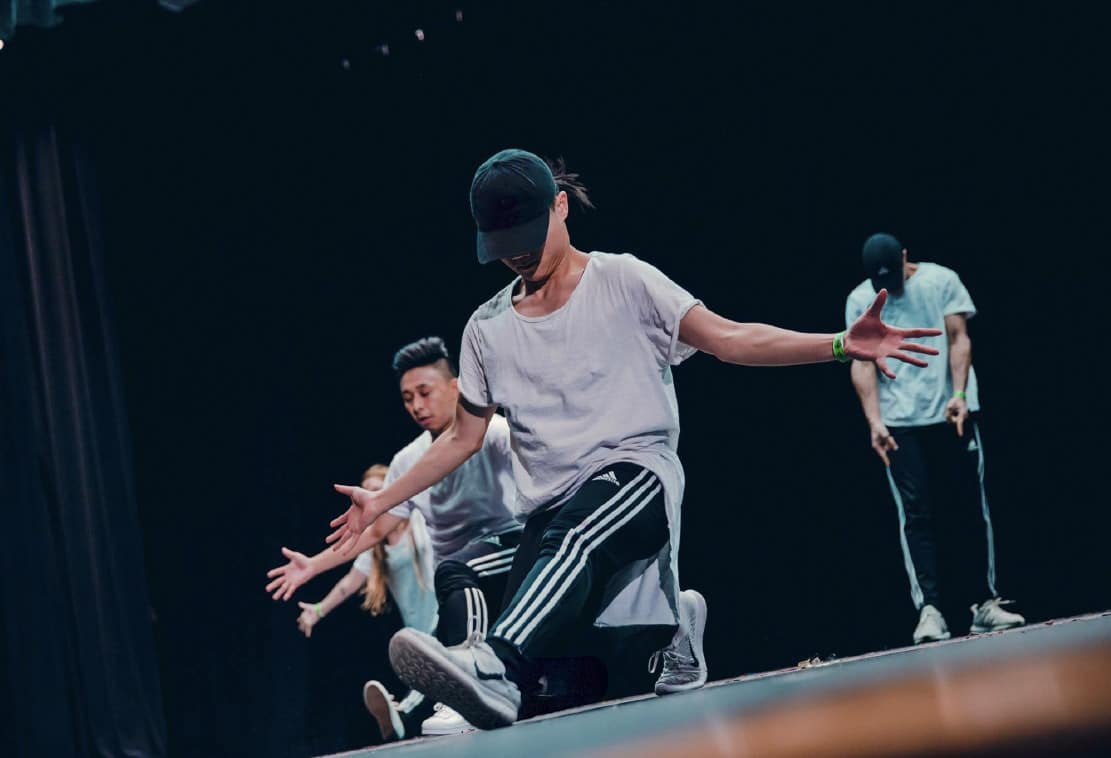
Kevin is a highly experienced dance physical therapist with over a decade of hands-on dance training and performance experience. Specializing in injury prevention and rehabilitation for dancers, he combines expert clinical care with a deep understanding of movement styles like hip hop, urban choreography, street jazz, and house.
He’s performed professionally—including on the BTS “Love Yourself” tour—and competed across the tri-state area, which gives him a unique edge when it comes to treating dancers. Kevin stays connected to the dance world by regularly taking class and choreographing, keeping his skills—and perspective—fresh.
His approach to physical therapy for dancers is rooted in whole-body wellness and tailored specifically to the demands of dance. Whether you're dealing with a dance-related injury, recovering from a performance, or just looking to move better and feel stronger, Kevin provides personalized care that helps dancers stay at their best.
